Understanding the Benefits of Online Urgent Care Services
Outline: What This Guide Covers
Before diving into details, this outline maps the terrain of online urgent care through the lenses of telemedicine, virtual consultations, and healthcare access. Each section builds on the last so you can understand not only how these services function, but also how they compare to walk-in clinics and what to do to get the most value from a visit. If you imagine urgent care as a busy intersection, telemedicine is the traffic system, virtual visits are the vehicles, and access is the open road that lets more people reach care without gridlock. Here is how the guide unfolds and what you can expect to take away from each part.
– Telemedicine fundamentals for urgent care: definitions, common clinical uses, benefits, limits, and safety considerations.
– Virtual consultation workflows: step-by-step visit flow, triage logic, documentation, privacy, and follow-up practices.
– Access and equity: who benefits, who risks being left out, and practical strategies to close gaps in connectivity, cost, and literacy.
– Quality and outcomes: what research tends to show about timeliness, patient satisfaction, and appropriate use of antibiotics, imaging, or referrals.
– Actionable takeaways: preparation checklists, when to switch to in-person care, and how to evaluate a service’s transparency and safeguards.
Throughout, you will find comparisons between online and in-person urgent care in terms of convenience, scope, and cost signals, with attention to clinical appropriateness. The goal is not to romanticize video calls, but to show how, when used thoughtfully, they can turn lost hours in a waiting room into minutes that genuinely matter. Expect plain-spoken explanations, a few reality checks, and plenty of practical pointers tailored to common urgent concerns such as rashes, sore throats, minor injuries, and medication questions.
Telemedicine in Urgent Care: Speed, Safety, and Scope
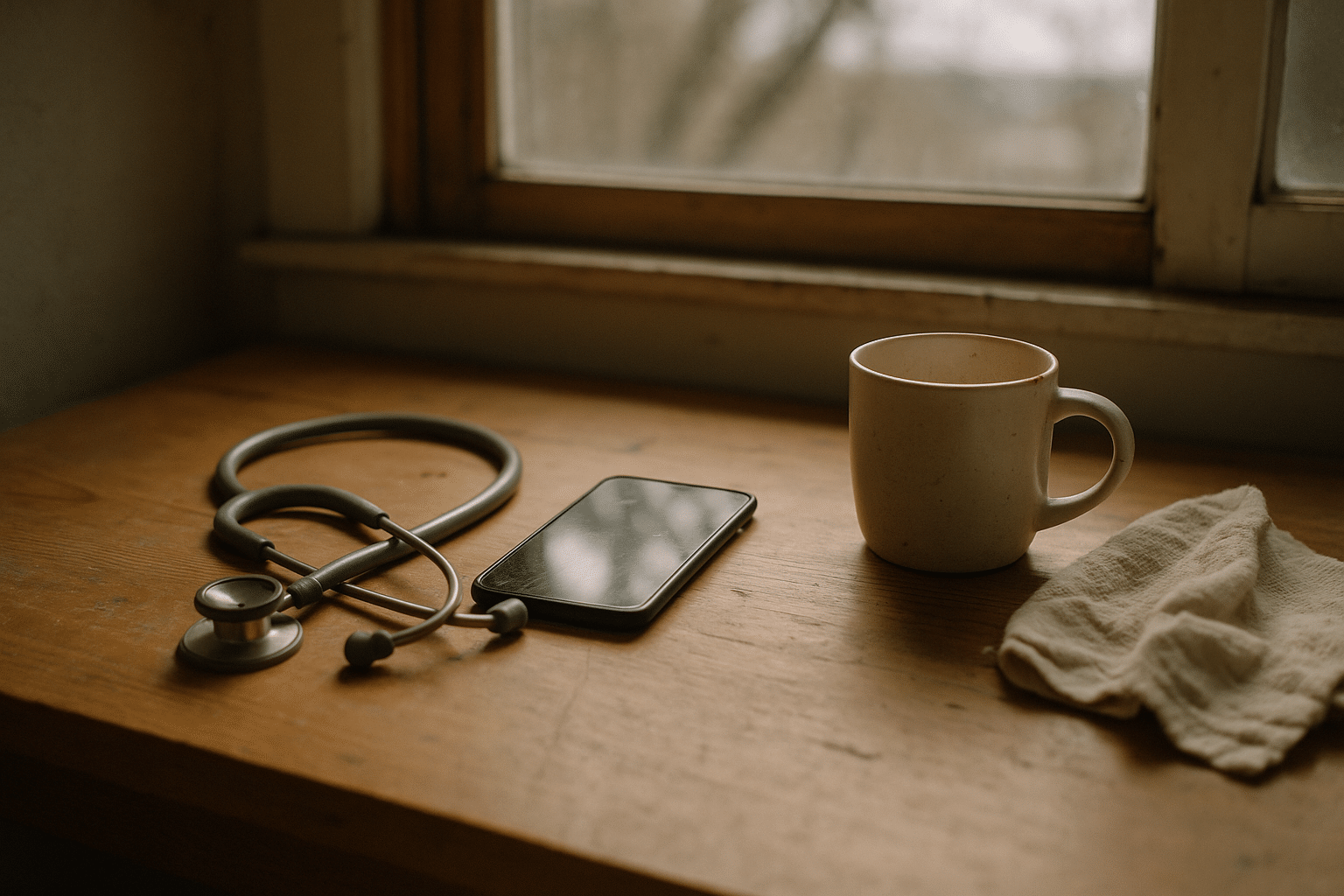
Telemedicine refers to delivering clinical care at a distance through digital tools, and in urgent care it usually means same-day access to a licensed clinician by video, audio, or secure messaging. Its value starts with time: instead of commuting, parking, and waiting, many people can connect from home or work and be triaged within minutes. During public health surges, usage climbed sharply across many health systems and, while it later stabilized, it remains substantially higher than pre-2020 levels. That endurance hints at a structural shift: patients and clinicians have found scenarios where remote care is efficient without sacrificing safety.
Scope is crucial. Online urgent care commonly handles problems where a careful history and visual assessment answer most of the clinical question. Examples include minor respiratory infections, uncomplicated urinary symptoms, skin conditions, red eye without vision changes, medication refills for stable needs, and guidance after a small cut or sprain. For these, clinicians can rule in or out warning signs, recommend over-the-counter options, prescribe when appropriate, and give clear self-care plans. Remote visits are less suitable when a hands-on exam, imaging, or procedures are likely. Chest pain, severe shortness of breath, major injuries, and symptoms of stroke remain emergencies that demand immediate in-person evaluation.
Comparisons with brick-and-mortar clinics show trade-offs rather than a single winner. Consider three dimensions: convenience, clinical completeness, and cost signals.
– Convenience: Online care shortens queues and reduces lost work time, especially in off-hours. In-person care consolidates assessment and tests in one place.
– Clinical completeness: Video offers visual cues but lacks palpation, vital sign measurement beyond home devices, or swabs unless pickup options exist.
– Cost signals: Many plans list lower copays or fees for virtual visits; patients also avoid travel and childcare expenses.
Safety depends on protocols. Reputable services use standardized triage questions to escalate urgent symptoms, maintain secure platforms, document thoroughly, and coordinate follow-up or referrals. When remote care defers a case to in-person evaluation, that is not failure; it is the system working as intended, ensuring the right care in the right setting.
Virtual Consultations: Tools, Triage, and the Patient Experience
A virtual consultation is the practical expression of telemedicine, turning software into a clinical visit. The visit begins before the call: you answer a brief intake that captures symptoms, duration, medications, allergies, and relevant history. Smart questionnaires flag red flags early, prompting the platform or clinician to advise urgent in-person care when needed. When a visit proceeds, video is preferred for visual cues—skin color, breathing effort, or a close look at a rash—while audio-only can work for straightforward concerns or low-bandwidth situations. Secure messaging is often used for follow-up, such as sharing care instructions or clarifying how to take a medication.
A smooth experience follows a predictable arc: intake, identity confirmation, consent, focused history, visual exam, differential diagnosis, shared decision-making, and a clear plan. Compare this with a walk-in clinic, and you notice the differences in what is measured and how. In-person visits routinely include vitals; virtual care may rely on your home thermometer, blood pressure cuff, or pulse oximeter if you have them. In return, virtual care often delivers faster starts, shorter total time, and easier access to same-day slots. The art is in matching the tool to the task: a sore throat with fever and no red flags can be evaluated by video, while a deep laceration clearly warrants a physical exam and possibly stitches.
Privacy and security are foundational. Platforms should encrypt data in transit, obtain explicit consent, and restrict recording unless transparently authorized. Clinicians document assessments and rationale just as they would in an exam room, ensuring continuity with your primary care record when possible. Practical preparation improves outcomes and satisfaction:
– Write down symptoms, onset, what helps or worsens them, and any exposures.
– Gather medications, allergies, and recent readings from home devices.
– Choose a quiet, well-lit spot; test your camera and microphone; ensure your device is charged.
– Keep a flashlight handy for throat or skin visualization if requested.
After the visit, you should receive a written summary with red flags to watch for, expected timelines for improvement, and how to seek follow-up. Clear instructions reduce unnecessary antibiotics, imaging, or repeat visits—a win for safety and cost alike.
Healthcare Access: Bridging Gaps with Digital Urgent Care
Access is where online urgent care can be quietly transformative. People in rural or remote areas often face long drives, limited clinic hours, or seasonal barriers like snowed-in roads. Workers with variable shifts or caregiving responsibilities may delay care because getting to a clinic is costly in time and logistics. For them, a same-day virtual slot can be the difference between early attention and a weekend of worsening symptoms. At the same time, access hinges on connectivity, devices, and digital literacy—gaps that can exclude the very communities telemedicine aims to serve.
Practical strategies help close these divides. Low-bandwidth options such as audio-only visits and photo uploads let patients participate even on unstable connections. Community libraries, clinics, and trusted organizations can host private telehealth rooms with reliable internet and support. Simple, multilingual interfaces, larger on-screen buttons, and plain-language summaries raise usability for people of varied literacy levels. Clear pricing pages reduce the fear of surprise bills, while transparent policies on privacy and data sharing build trust, especially for those new to remote care.
Equity also involves clinical scope. Conditions that have strong visual cues—like dermatologic concerns—translate well to video when instructions are clear and images are well lit. Mild respiratory symptoms or medication questions are similarly accessible. But for high-stakes, low-tolerance problems, online urgent care should serve as a guidepost rather than a destination, pointing swiftly to hands-on evaluation. Programs that blend virtual triage with convenient in-person testing, mobile units, or rapid referral pathways create a continuum that meets patients where they are.
Consider three access levers you can look for when evaluating a service:
– Flexible modalities: video, audio-only, and messaging for follow-up, chosen based on your bandwidth and comfort.
– Clear pathways: explicit steps to escalate to local in-person care, including maps, hours, and realistic timelines.
– Supportive design: language options, readability features, and upfront fee estimates to limit financial surprises.
When these pieces align, online urgent care doesn’t just make care faster; it makes it reachable for people who previously had little to no timely option.
Conclusion: Choosing and Using Online Urgent Care Wisely
If you are considering online urgent care, think of it as a tool that works best when aimed precisely. It excels at quick guidance for common, uncomplicated issues and at answering the immediate question, “Do I need to be seen in person today?” To use it well, prepare briefly before you connect, be honest and specific about symptoms, and keep a low threshold for switching to in-person care if red flags appear. No video call replaces an emergency department for severe chest pain, difficulty breathing, heavy bleeding, or neurologic symptoms; in those cases, seek emergency help without delay.
To get practical value from your first or next visit, try this short checklist:
– Note symptom timing, severity, and triggers; list medications and allergies.
– Have home measurements ready if available: temperature, blood pressure, heart rate, oxygen saturation.
– Ensure a steady internet connection; if bandwidth is limited, request audio with photo uploads.
– Ask three key questions at the end: what is the likely diagnosis, what should I do if I worsen, and when should I expect to feel better?
As you compare services, look for signs of thoughtful design: clear pricing, explicit privacy practices, clinician credentials, and realistic scope statements that explain what they can and cannot do remotely. Services that prominently state limitations—and provide direct pathways to in-person care—signal maturity and patient-centered values. For ongoing needs, consider linking your urgent care account to your primary care record when that option exists; continuity helps avoid duplicated tests and medication conflicts.
Online urgent care, grounded in telemedicine and delivered through virtual consultations, is not a magic wand, but it is a remarkably practical wrench in the healthcare toolbox. Used thoughtfully, it can save hours, reduce costs associated with travel and time away from work, and get you timely reassurance or escalation when it matters most. Approach it with preparation and curiosity, and you will be well-positioned to turn a quick digital check-in into meaningful, safe care.